Emergency departments (EDs) across the United States handle over 130 million visits annually. From car accidents to cardiac arrest, the ER is where lives are stabilized, diagnoses are clarified, and rapid treatment decisions are made under pressure. While the system is built to save lives, it is also one of the most overburdened and misunderstood parts of healthcare.
This article breaks down how emergency care operates, what to expect during a visit, what conditions are treated first, and how hospitals prioritize care with limited resources.
Average ER Wait Time by Emergency Condition
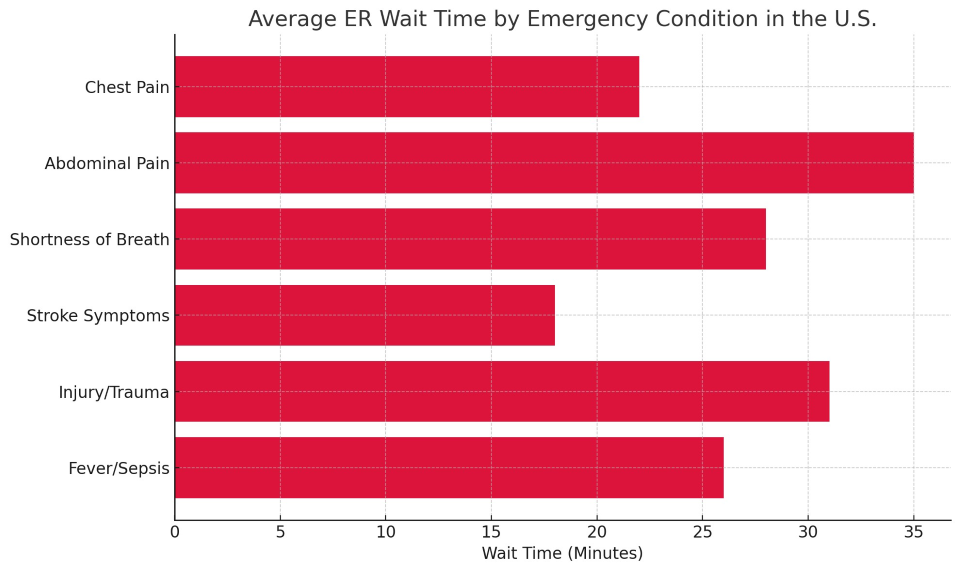
As the chart shows, patients with life-threatening symptoms like stroke or chest pain are treated significantly faster than those with symptoms like abdominal pain or trauma injuries, which may be less urgent upon initial assessment.
What Qualifies as Emergency Care?
Emergency care is defined as immediate medical intervention for symptoms or injuries that pose a serious threat to health, life, limb, or long-term function if not treated quickly. These services are available 24/7, regardless of a patient’s ability to pay, thanks to the federal EMTALA law (Emergency Medical Treatment and Labor Act).
Conditions that require emergency care:
-
Severe chest pain or suspected heart attack
-
Difficulty breathing or sudden shortness of breath
-
Stroke symptoms (e.g., one-sided weakness, facial droop)
-
Serious trauma or injuries (car accidents, gunshot wounds)
-
Uncontrolled bleeding
-
Loss of consciousness or seizures
-
High fever with confusion (possible sepsis)
While many people seek emergency care for non-urgent reasons, hospitals triage every patient to ensure critical cases receive care first.
Understanding Triage: Why Some People Wait Longer
When you arrive at an ED, you're assessed by a triage nurse, who determines the urgency of your condition. Hospitals typically use a five-level triage scale:
-
Level 1 – Resuscitation: Life-threatening (e.g., cardiac arrest)
-
Level 2 – Emergent: High risk of deterioration (e.g., stroke)
-
Level 3 – Urgent: Moderate risk (e.g., abdominal pain)
-
Level 4 – Less urgent: Low risk (e.g., minor injury)
-
Level 5 – Non-urgent: Very low risk (e.g., medication refill)
This system means someone who arrived after you may be seen first if their condition is more critical.
Inside the Emergency Department: Who's on the Team
The ER is staffed by a multidisciplinary team trained to handle time-sensitive decisions:
-
Emergency physicians (board-certified)
-
Registered nurses (RNs) with trauma or emergency training
-
Respiratory therapists
-
Radiology techs for immediate imaging
-
Laboratory personnel
-
On-call specialists (neurology, trauma surgery, cardiology)
-
Security and mental health responders
In larger trauma centers, stroke teams and STEMI (heart attack) protocols can activate full units within seconds.
A Real Patient Scenario
Patient: Angela, 62, arrives with slurred speech and confusion
Triage result: Level 2 – Possible stroke
Action: CT scan within 12 minutes, neurology consult in 15
Diagnosis: Ischemic stroke
Treatment: tPA administered in under 40 minutes
Angela walks out of the hospital 4 days later with no permanent disability. This is emergency care at its best—swift, effective, and life-changing.
Costs and Access: What You Need to Know
Emergency care is expensive, particularly for the uninsured:
-
Basic ER visit (no tests): $500–$1,200
-
With imaging and labs: $2,000–$4,000
-
Ambulance transport: $500–$1,500
-
Trauma activation: $10,000+
If you’re uninsured or underinsured, you will still be treated, but you may receive a large bill. Ask about charity care or hospital financial assistance before leaving the facility.
How Emergency Departments Differ from Urgent Care
Use urgent care for flu symptoms, minor infections, or small injuries. Use the ER when something feels serious—or when your life might depend on it.
Emergency Room Overuse: A National Problem
Many Americans turn to the ER for non-urgent issues, often because:
-
They lack primary care access
-
They don’t have insurance
-
Clinics aren’t open after hours
-
They are uncertain if the issue is serious
This clogs ER resources, leads to longer waits, and increases healthcare costs overall. States and hospitals are investing in:
Technology in Modern Emergency Medicine
Emergency care is evolving with:
-
AI-powered triage algorithms
-
Mobile stroke units with on-board CT scans
-
Digital dashboards for capacity management
-
Telehealth within the ED for quick access to remote specialists
-
Patient tracking tools to notify families in real time
Hospitals using these tools report better patient flow and fewer “left without being seen” incidents.
Emergency care in the U.S. is a lifeline, a safety net, and often, the starting point for long-term recovery. While it isn’t perfect—plagued by rising costs and long wait times—its value is indisputable. Understanding how emergency services work can empower you to make smarter, faster decisions during life’s most stressful moments.
When time matters most, the ER is where help begins.