Internal medicine—often called the heart of adult care—is a cornerstone of the American healthcare system. Internists, the physicians who specialize in this field, serve as primary care providers for adults and play a vital role in preventing hospitalizations, managing chronic illnesses, and coordinating with specialists. In a country where chronic conditions are rising and healthcare systems are stretched thin, internists are more essential than ever.
This article explores the full scope of internal medicine: what it includes, how internists are trained, where they work, and why demand for their expertise is surging.
What Is Internal Medicine?
Internal medicine focuses on diagnosing, treating, and preventing non-surgical diseases in adults. Internists are trained to handle both common illnesses and complex medical conditions, often treating multiple issues at once. They don’t perform surgery, but they coordinate care with other specialists, making them central to a patient’s long-term health journey.
Conditions Managed:
-
Diabetes and hypertension
-
Heart disease
-
Kidney and liver disorders
-
Respiratory conditions (e.g., asthma, COPD)
-
Thyroid and endocrine disorders
-
Infectious diseases
-
Gastrointestinal and autoimmune diseases
Internists manage patients in both outpatient clinics and hospital settings, depending on their subspecialty or work environment.
Internal Medicine vs. Family Medicine
Though both fields provide primary care, there are important distinctions:
Internists are often the go-to physicians in hospitals and for patients with multiple chronic conditions requiring ongoing care coordination.
Education and Subspecialty Pathways
Internists must complete:
-
4 years of medical school
-
3 years of internal medicine residency
-
Optional 2–3 years of fellowship training for subspecialties
Common Subspecialties:
-
Cardiology
-
Gastroenterology
-
Endocrinology
-
Nephrology
-
Pulmonology
-
Rheumatology
-
Hematology/Oncology
Each subspecialty brings additional complexity, requiring board certification and ongoing education to stay up to date with evolving medical standards.
Internists and the Bigger Picture: Public Health & Prevention
Internal medicine doctors don’t just treat individuals—they shape public health outcomes. Many internists are involved in:
-
Vaccination programs
-
Health screenings (cholesterol, cancer, diabetes)
-
Lifestyle intervention counseling
-
Managing social determinants of health
By emphasizing preventive care, internists help reduce hospital admissions and long-term healthcare costs.
Collaboration Across the Care Spectrum
Internists work in multidisciplinary teams and frequently collaborate with:
-
Pharmacists for medication management
-
Nurses and nurse practitioners for follow-ups and chronic care
-
Social workers for addressing mental health and housing issues
-
Specialists for managing organ-specific conditions
They are often the first to recognize when a patient’s care plan is too fragmented or inefficient—and step in to streamline it.
Trends: Visit Volume and Physician Demand
The numbers reflect an upward trend in both patient visits and physician demand, especially in the wake of COVID-19 and delayed care.
Internal Medicine Trends in the U.S.
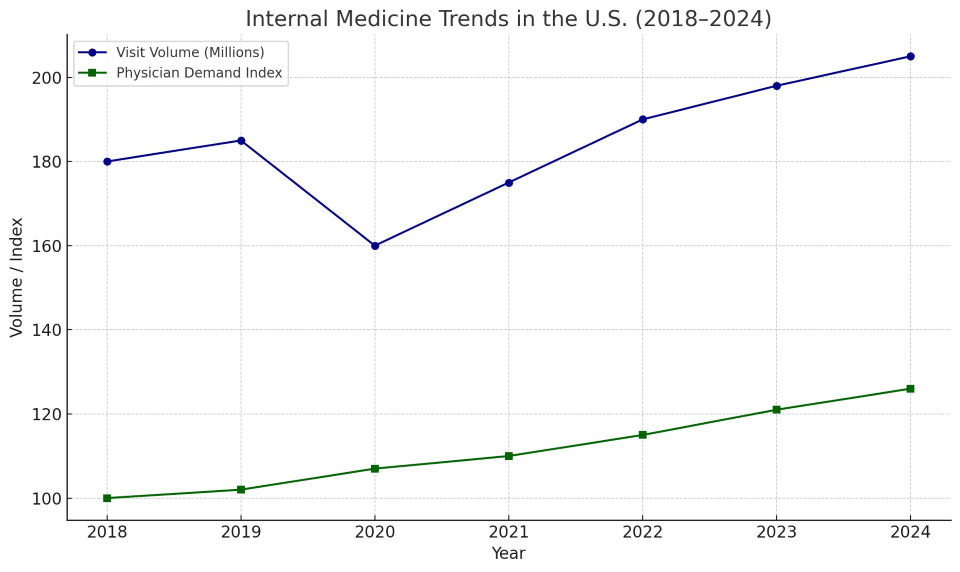
This line chart shows the rising visit volume and growing physician shortage, highlighting a specialty that is both overloaded and under-resourced.
Internists in Action: A Real-World Example
Patient: James, 70, with diabetes, high blood pressure, and early-stage kidney disease
Internist’s Role:
-
Orders and interprets labs
-
Adjusts multiple medications
-
Coordinates care with a nephrologist and cardiologist
-
Counsels on diet and exercise
-
Tracks patient progress every 3 months
Without this ongoing internal medicine support, James would likely face frequent ER visits and hospital stays.
Technology and the Future of Internal Medicine
Internists are embracing technology to improve access and outcomes. Key tools include:
-
Remote patient monitoring for blood pressure and glucose
-
AI-powered diagnostic tools to catch early signs of disease
-
EHR integration with decision support
-
Patient portals for scheduling, communication, and records
In rural or underserved communities, telemedicine has become especially crucial, helping internists reach patients who would otherwise go untreated.
Workforce Crisis: Burnout and Shortage
According to the AAMC, the U.S. may face a shortage of up to 55,000 primary care physicians by 2035, many of them internists.
Causes:
-
Administrative overload (EHR documentation, billing)
-
Lower compensation compared to specialists
-
Fewer medical graduates choosing internal medicine as a long-term path
Potential Solutions:
-
Loan repayment incentives for primary care
-
Team-based care models to share the workload
-
Expanded roles for PAs and NPs
-
Value-based payment systems that reward outcomes, not volume
Policy Implications: Internists at the Center of Reform
Internal medicine is central to healthcare reform efforts focused on:
-
Reducing hospital readmissions
-
Lowering chronic disease costs
-
Expanding access in rural areas
-
Improving care continuity for seniors
Federal programs like Medicare Shared Savings (ACOs) and Chronic Care Management (CCM) directly involve internists in reducing waste and improving care delivery.
Internal medicine is more than a specialty—it’s the strategic command center of adult healthcare. Internists are uniquely trained to see the big picture, manage the details, and guide patients through every stage of their health journey.
As healthcare shifts toward more preventive, value-based, and coordinated models, internal medicine will remain not just relevant—but indispensable.