Home-Based Primary Care (HBPC) is transforming healthcare in the United States, offering an innovative and compassionate alternative to traditional office-based medicine. By delivering primary care services directly to a patient’s residence, this model ensures ongoing, personalized care for individuals who are homebound, medically complex, or managing multiple chronic illnesses.
This article explores HBPC from every angle: what it is, how it works, who it serves, and why it matters. We'll also look at trends, technology, policy, and challenges, all through the lens of the U.S. healthcare system.
What Is Home-Based Primary Care?
HBPC brings comprehensive, longitudinal primary care directly to the homes of patients. It goes far beyond short-term post-hospital nursing care. Instead, it functions like a primary care practice—delivering everything from routine physicals to end-of-life care—all in the patient’s living room.
HBPC often includes:
-
Preventive care and health screenings
-
Chronic disease management
-
Medication adjustments
-
Lab testing and imaging (via mobile services)
-
Mental health assessments
-
Care coordination and referrals
Unlike standard home health, HBPC is managed by an interdisciplinary team of doctors, nurse practitioners, nurses, social workers, and sometimes mental health professionals, all working together to provide holistic care.
Who Benefits from HBPC?
The target population includes:
-
Seniors with mobility limitations
-
Patients with multiple chronic conditions (e.g., diabetes, heart failure, COPD)
-
Individuals with cognitive impairments (e.g., Alzheimer’s, dementia)
-
Recently discharged patients at high risk of readmission
-
Those lacking access to transportation or caregiver support
According to the Centers for Medicare & Medicaid Services (CMS), more than 2 million Americans are “permanently homebound,” meaning they cannot leave their home without considerable effort or assistance. This is the core population HBPC aims to serve.
Case Example: HBPC in Practice
Patient: Mr. Allen, a 78-year-old retired teacher with advanced heart failure and Type 2 diabetes.
Before HBPC: Multiple ER visits every 2–3 months, missed appointments, medication confusion, caregiver burnout.
After HBPC Enrollment:
-
A nurse visits weekly to monitor vitals and adjust meds.
-
A social worker helps coordinate meal delivery and mobility aids.
-
A doctor visits monthly and manages labs and specialist referrals.
Results: Mr. Allen hasn’t had an ER visit in 9 months. His A1C has improved, and his daughter (primary caregiver) reports reduced stress and better work-life balance.
This is just one of thousands of similar stories across the country.
Cost and Outcome Comparison
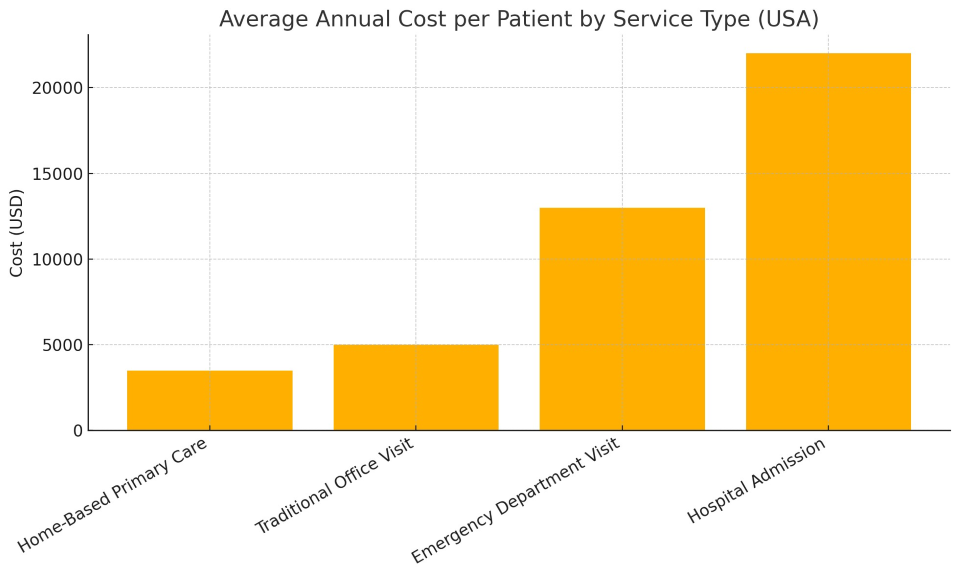
The chart and table below show the average annual cost per patient and hospital readmission rates across different care settings in the U.S.:
This data supports what many HBPC programs have found in practice: providing high-quality, patient-centered care at home can significantly reduce both healthcare costs and complications.
Benefits of Home-Based Primary Care
1. Improved Access
Many HBPC patients would otherwise go without care due to transportation, cognitive, or mobility barriers. HBPC reduces that gap.
2. Better Patient Outcomes
Studies show lower rates of hospitalization, improved medication adherence, and higher satisfaction among HBPC patients compared to traditional care.
3. Cost Savings
Programs like VA HBPC and CMS's Independence at Home Demonstration have shown 20–30% cost savings by reducing ER use, hospitalizations, and complications.
4. Personalized, Relationship-Driven Care
Unlike rushed clinic visits, HBPC providers often spend 30–60 minutes with patients, fostering trust and catching problems early.
Technology Enabling HBPC
The growth of HBPC has been fueled by advances in mobile health tech. Key tools include:
-
Portable diagnostic devices: ECGs, glucose monitors, portable X-ray and ultrasound equipment
-
Remote patient monitoring (RPM): Devices that send blood pressure, oxygen, and weight data to providers in real time
-
Telehealth integration: Virtual consults supplement in-person visits, especially for mental health
-
Electronic health records (EHRs): Mobile EHRs allow real-time documentation from the patient's home
How HBPC Fits into U.S. Healthcare Policy
Medicare and Medicaid Coverage
-
Medicare: Covers HBPC through providers who accept Part B and participate in approved demonstration programs (e.g., Independence at Home).
-
Medicaid: Varies by state. Some states offer strong support through Managed Long-Term Services and Supports (MLTSS) or PACE (Program of All-Inclusive Care for the Elderly).
-
Veterans Affairs (VA): Operates the most robust HBPC model, serving tens of thousands of veterans in all 50 states.
Workforce and Training Challenges
While HBPC is growing, scaling it remains difficult due to workforce limitations:
-
Shortage of trained providers comfortable practicing independently in the home setting
-
Burnout and isolation risk for providers working solo in the field
-
Lack of standardized training pathways, although programs like Home Centered Care Institute (HCCI) are trying to fill the gap
Addressing Health Disparities
HBPC has the potential to reduce healthcare inequality. Populations that are traditionally underserved—such as low-income seniors, rural residents, and disabled individuals—are often those who benefit most from in-home care.
Because HBPC providers see patients in their real environments, they often detect issues missed in clinic settings, such as:
Future of HBPC: Where Is It Heading?
-
Expansion of tele-home models blending in-person and virtual visits
-
Integration with ACOs (Accountable Care Organizations) for shared savings and care coordination
-
Bundled payment models to incentivize holistic outcomes over service volume
-
Greater focus on mental health services delivered at home
-
Increased funding from CMS as part of value-based care initiatives
The goal is to make HBPC not just a niche solution, but a scalable, system-wide standard for complex, homebound patients.
Home-Based Primary Care is reshaping what it means to “go to the doctor.” Instead of bringing the patient to care, HBPC brings care to the patient—safely, efficiently, and with a level of personal connection that traditional systems often lack.
As the American population ages and the burden of chronic illness grows, HBPC offers a sustainable, humane, and smart way to keep people healthy and out of hospitals. It's not just an option—it’s part of the solution.