Medical physics is a specialized branch of applied physics focused on the use of radiation and imaging technologies in healthcare. It combines physics, biology, and engineering to improve diagnosis, treatment, and patient safety. In the United States, medical physicists are essential to the infrastructure of hospitals and cancer treatment centers, working mostly behind the scenes to make sure high-stakes medical procedures are accurate, safe, and effective.
Despite being relatively unknown outside the healthcare industry, medical physicists are vital. They help run complex systems that many physicians rely on—such as MRI, CT, X-ray, PET, and radiation therapy machines—ensuring that these systems deliver precise results that could determine the outcome of a patient’s treatment.
What Do Medical Physicists Actually Do?
Medical physicists apply their expertise in a few core areas:
-
Radiation Therapy (Therapeutic Medical Physics): Planning and verifying the accurate delivery of radiation to cancerous tissues, minimizing harm to surrounding healthy tissue.
-
Diagnostic Imaging (Diagnostic Medical Physics): Ensuring that imaging devices (MRI, CT, mammography, ultrasound) are working properly and producing high-quality, reliable images.
-
Nuclear Medicine Physics: Supporting the use of radioactive substances for diagnosis and treatment, such as PET scans or radioisotope therapy.
-
Radiation Safety (Health Physics): Monitoring radiation use and ensuring that patients, staff, and the public are protected from unnecessary exposure.
Every time a radiation therapy machine is used to treat cancer, or a diagnostic image is taken to help identify disease, a medical physicist has been involved in calibrating and maintaining that system.
Breaking Down the Specialties
To better understand where medical physicists work and what they do, here’s a detailed breakdown:
(Refer to the interactive table titled “Medical Physics Roles and Settings” above.)
These roles aren't just technical—they’re clinical. Physicists work with oncologists, radiologists, and other healthcare professionals to plan procedures and treatment paths tailored to each patient.
Role in the U.S. Healthcare System
In the U.S., more than 1.9 million new cancer cases are expected each year. About half of those patients will receive some form of radiation therapy. With so many procedures relying on accurate and safe radiation delivery, the demand for medical physicists remains high.
Beyond oncology, diagnostic imaging is a massive component of modern healthcare. Every day, tens of thousands of CT scans, MRIs, and X-rays are performed across U.S. hospitals. Medical physicists are the experts who make sure these machines are calibrated, tested, and working under optimal, FDA-compliant conditions.
Furthermore, the U.S. health system is deeply regulated. Institutions must comply with standards from the:
Medical physicists are often the go-to personnel for meeting and documenting compliance with these regulations, particularly regarding radiation use and safety.
Supply vs. Demand: A Growing Gap
The number of board-certified medical physicists in the U.S. hovers around 4,500. However, healthcare demand is rising—driven by an aging population, higher cancer incidence, and increased imaging use. Unfortunately, training programs aren’t keeping up, and many current physicists are approaching retirement.
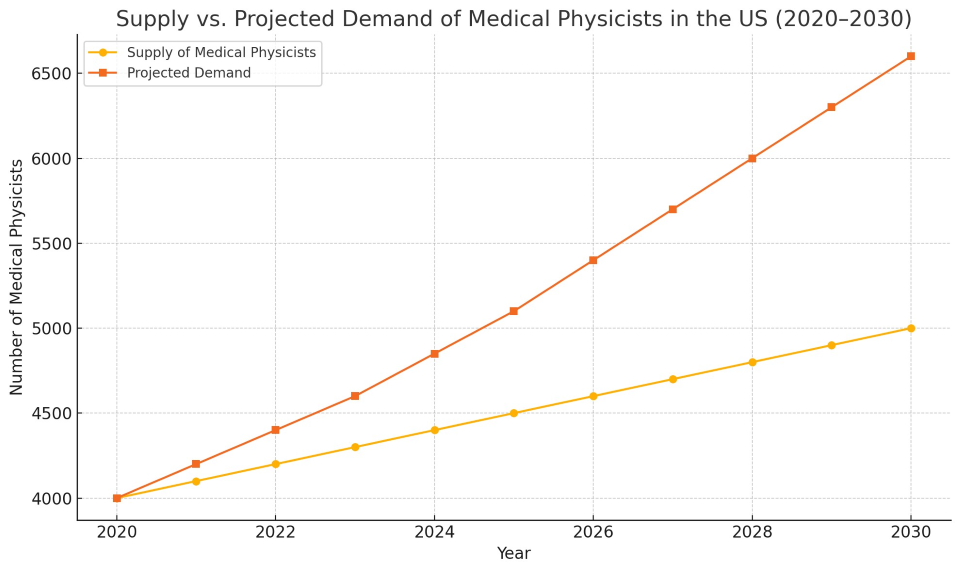
As shown in the graph, the supply of new professionals isn’t expected to meet projected needs through 2030. Rural hospitals, in particular, struggle to recruit and retain physicists, leading to unequal access to high-quality care.
Education and Certification
To become a clinical medical physicist in the U.S., candidates must go through a rigorous path:
-
Bachelor’s Degree: Usually in physics or a related discipline.
-
Graduate Degree: Master’s or PhD in medical physics from a CAMPEP-accredited program.
-
Clinical Residency: A 2-year residency focusing on clinical experience.
-
Board Certification: Administered by the American Board of Radiology (ABR) or American Board of Medical Physics (ABMP). This involves written and oral exams covering physics principles, clinical practice, and safety standards.
Some physicists go on to specialize further, perform academic research, or take leadership roles in hospital systems.
|
Medical Physics Specialty |
Typical Work Setting |
Primary Responsibilities |
|
Radiation Oncology Physics |
Cancer treatment centers, hospitals |
Ensure accurate radiation dose delivery in cancer treatments, equipment calibration, treatment planning |
|
Diagnostic Imaging Physics |
Radiology departments, imaging centers |
Maintain image quality and radiation safety in diagnostic procedures like CT, MRI, X-ray |
|
Nuclear Medicine Physics |
Hospitals, PET centers, research labs |
Oversee use and safety of radiopharmaceuticals, quality control of imaging equipment |
|
Health Physics (Radiation Safety) |
Hospitals, regulatory bodies, universities |
Monitor radiation levels, implement safety protocols, ensure regulatory compliance |
Real-World Impact: Where Physics Meets People
Though they rarely interact directly with patients, the work of a medical physicist has a direct human impact.
-
Example 1: In radiation therapy, a physicist helps tailor treatment plans so that a tumor receives a lethal dose of radiation without damaging nearby organs. A one-millimeter error could mean serious complications or reduced effectiveness.
-
Example 2: In imaging, they test and fine-tune systems so that a CT scan delivers minimal radiation but still detects a small tumor. This helps doctors catch diseases earlier without overexposing the patient.
This invisible hand behind care is why many physicians call medical physicists “the unseen safety net” of modern medicine.
Challenges Ahead
While the profession is rewarding and intellectually rich, it’s not without obstacles:
-
Burnout and Workload: Especially in smaller hospitals, a single physicist may be responsible for dozens of machines and thousands of procedures.
-
Technological Complexity: Systems are becoming more advanced, requiring physicists to continuously retrain.
-
Shortage of Residency Slots: There are more graduates than available clinical residency spots, which slows down entry into the field.
Organizations like the American Association of Physicists in Medicine (AAPM) are actively advocating for policy changes, better funding, and more educational opportunities.
Looking Forward
As healthcare continues to evolve with AI, precision medicine, and new forms of radiotherapy (e.g., proton and heavy ion therapy), medical physicists will be essential in ensuring that these tools are safe and effective.
Investing in training, recruiting, and retaining medical physicists isn’t just about staffing—it’s about patient outcomes. When this layer of safety and precision is compromised, the whole system risks faltering.
Medical physics isn’t a flashy field. You won’t see it dramatized in medical shows. But behind every precise cancer treatment, every clean diagnostic image, and every safe use of radiation, a medical physicist is making it happen.
In a healthcare system as vast and technologically advanced as the U.S., their role is not just important—it’s indispensable.