Pain is one of the most common reasons Americans seek medical attention. Whether it's due to injury, chronic illness, surgery, or age-related conditions, pain affects more than 50 million U.S. adults every year. But how that pain is managed has evolved dramatically—especially in response to the opioid crisis, healthcare innovation, and a growing push for personalized care.
In this article, we’ll break down the current landscape of pain management in the U.S., exploring therapy types, usage rates, effectiveness, and real-world trends. Plus, we’ll look at the data: what’s working, what’s overused, and what’s emerging.
What Is Pain Management?
Pain management refers to a range of medical and therapeutic approaches aimed at reducing or controlling pain, improving quality of life, and increasing functionality. It includes everything from over-the-counter drugs and physical therapy to advanced surgical implants and psychological support.
Pain is generally classified into two types:
-
Acute pain: Sudden onset, usually after injury or surgery.
-
Chronic pain: Persists for 3+ months, often due to conditions like arthritis, fibromyalgia, or nerve damage.
Effective pain management often requires a multimodal approach, combining multiple therapies tailored to the individual.
The Landscape of Pain Therapies in the U.S.
Below is a breakdown of the most widely used pain management therapies in the country:
Most Common Pain Management Therapies
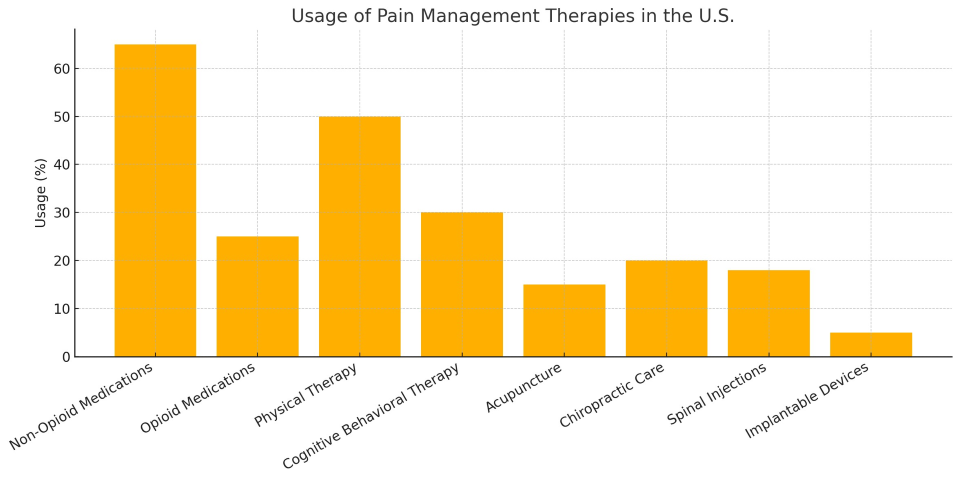
The chart above shows how common each pain therapy is in the U.S. Non-opioid medications (like NSAIDs and acetaminophen) are the most used, while implantable devices are rare but highly effective for select cases.
Detailed Overview of Key Therapies
1. Non-Opioid Medications
These include over-the-counter options such as ibuprofen and acetaminophen. They’re often the first line of defense for mild to moderate pain. They’re widely available and generally safe when used correctly but can pose risks if overused (e.g., liver or kidney damage).
2. Opioid Medications
Reserved for severe pain—especially post-surgery or cancer-related pain—opioids like oxycodone and morphine are effective but come with high addiction potential. Prescribing guidelines have tightened significantly since the opioid crisis, and long-term use is discouraged.
3. Physical Therapy
A non-invasive, high-impact solution for pain related to musculoskeletal issues, surgery recovery, or mobility problems. It improves strength, flexibility, and alignment. Many chronic pain patients benefit more from consistent PT than from medication alone.
4. Cognitive Behavioral Therapy (CBT)
Pain isn’t just physical—it’s emotional and psychological, too. CBT helps patients change negative thought patterns and improve coping strategies. It’s especially effective for chronic pain linked to depression or anxiety.
5. Acupuncture
An ancient practice that involves inserting thin needles into specific body points. Modern research supports its use in treating conditions like back pain, migraines, and osteoarthritis. It's low-risk, but effectiveness varies between individuals.
6. Chiropractic Care
Focuses on manual adjustments, especially of the spine. Widely used for lower back and neck pain. While controversial in some circles, many patients report meaningful pain relief with regular visits.
7. Spinal Injections
Includes epidural steroid injections and nerve blocks. These are typically used for localized back or joint pain and can offer fast, temporary relief. Often used alongside PT or surgery planning.
8. Implantable Devices
These include spinal cord stimulators or intrathecal pain pumps. They’re used in very advanced cases where other therapies have failed. While costly and invasive, they offer life-changing benefits for certain patients with neuropathic or intractable pain.
Trends and Innovations in Pain Management
Pain care is rapidly evolving. Here’s what’s changing:
-
Personalized Pain Plans: Doctors increasingly combine therapies based on patient genetics, pain type, lifestyle, and mental health.
-
AI and Wearables: Smart devices track pain episodes and trigger patterns, offering real-time insights to doctors.
-
Non-Addictive Analgesics: Research is booming in non-opioid medications targeting specific pain receptors.
-
Virtual Pain Clinics: Telehealth platforms now offer CBT, PT coaching, and pain tracking remotely—especially useful for rural patients.
Challenges in Pain Care
Despite the innovations, the system isn’t perfect. Key challenges include:
-
Access to specialists: Pain medicine is a specialized field, and many rural areas lack trained practitioners.
-
Insurance coverage: Alternative therapies like acupuncture or behavioral therapy are often not fully covered.
-
Stigma: Patients with chronic pain, especially those requiring opioids, often feel judged or dismissed.
-
Fragmented care: Pain treatment often requires coordination across multiple specialists—something many systems struggle to deliver.
The U.S. is still recovering from the opioid epidemic, and pain treatment is at the center of that conversation. New CDC guidelines emphasize:
-
Trying non-opioid options first
-
Limiting doses and duration
-
Close monitoring for chronic use
This has led to a cultural shift in how both doctors and patients approach pain—away from “quick fixes” and toward long-term, integrated care.
Pain is deeply personal, and no single solution fits all. From physical therapy to psychological support, injections to innovation, the landscape of pain management in the U.S. is broad and growing. The best outcomes often come from combining therapies and treating the whole person—not just the symptom.
If you or someone you love is living with chronic or acute pain, know that there are options. Talk to your healthcare provider about creating a personalized plan, and don’t be afraid to explore therapies beyond pills.