Mental health is a critical part of healthcare, yet it’s often the most neglected. In the United States, millions struggle with depression, anxiety, substance use, or trauma—but only a portion receive consistent support. As awareness grows, the systems meant to provide care are being tested like never before.
This article breaks down the structure of mental health services, most-used care types, access challenges, and the growing role of technology and public policy in meeting mental health needs across the country.
Mental Health Services Usage Rates
Mental Health Services Usage in the U.S.
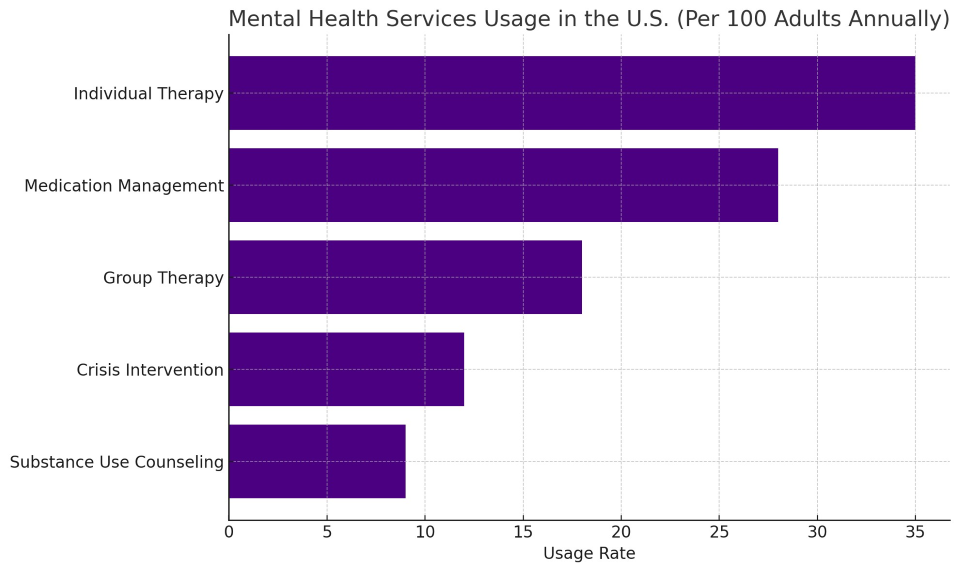
The data shows how therapy and medication remain the most common forms of mental health support, while group programs and crisis services are less utilized, often due to limited availability or long waitlists.
What Falls Under Mental Health Services?
Mental health services include professional and community-based care that support emotional, psychological, and behavioral wellbeing. These services are offered through:
-
Private therapy offices
-
Community clinics
-
Hospitals and emergency departments
-
Primary care offices
-
Online platforms
-
Schools, churches, and shelters
Services aim to address a wide range of conditions including anxiety, depression, PTSD, bipolar disorder, schizophrenia, substance abuse, grief, and adjustment disorders.
Key Providers in the Mental Health System
These professionals work in coordination when possible, especially for individuals with multiple or severe mental health needs.
Main Types of Services People Use
1. Individual Therapy
The foundation of mental healthcare. Individuals meet one-on-one with a therapist to work through personal challenges, mental illness, or emotional trauma.
2. Medication Management
Psychiatrists or primary care doctors prescribe and monitor antidepressants, anti-anxiety meds, or mood stabilizers. Adjustments depend on response and side effects.
3. Group Therapy
Led by a clinician, these sessions provide structured peer support for shared challenges like grief, anger management, addiction, or anxiety.
4. Crisis Intervention
Immediate help for people in mental health emergencies. Includes suicide prevention hotlines, mobile crisis units, and psychiatric ER services.
5. Substance Use Counseling
Focused therapy for alcohol, drug, or behavioral addictions. Often combined with detox support or Medication-Assisted Treatment (MAT).
Case Example: Long-Term Recovery Through Combined Care
Patient: Nicole, 36, struggling with panic attacks and sleep issues
Treatment Plan:
-
Weekly cognitive behavioral therapy
-
Low-dose anti-anxiety prescription
-
Sleep hygiene coaching
-
Two-month group program for emotional regulation
Result: After 6 months, symptoms decreased significantly, with no emergency room visits since starting care. Nicole credits regular therapy and having a provider who understood her history.
Barriers That Keep People From Getting Help
Despite growing demand, many Americans still face major obstacles:
1. Cost
Even with insurance, co-pays for therapy or psychiatry can be high. Without coverage, a single session can cost $100–$250.
2. Provider Shortages
Over 150 million people in the U.S. live in areas with a shortage of mental health professionals. Wait times for new patients can stretch to 2–3 months.
3. Social Stigma
Fear of judgment or being labeled “unstable” prevents people from seeking care, especially older generations and those in conservative regions.
4. Inconsistent Coverage
Some insurance plans limit the number of therapy visits or exclude specific medications or types of care like telehealth or family therapy.
Mental Health at Work and School
Organizations are recognizing the role of mental health in performance and learning:
In the Workplace:
-
Employers now offer Employee Assistance Programs (EAPs)
-
Mental health days and flexible schedules are more common
-
Corporate partnerships with therapy platforms have grown
In Schools:
-
More districts are embedding school counselors and therapists
-
Education on coping skills and emotional intelligence is expanding
-
Partnerships with local clinics help connect families to support
These settings provide a first line of detection and referral for issues that might otherwise go unnoticed.
Community-Based and Government Resources
Not everyone can afford private care. Fortunately, there are public and nonprofit resources:
-
Federally Qualified Health Centers (FQHCs) offer sliding-scale therapy
-
County crisis lines offer 24/7 support
-
The 988 National Suicide & Crisis Lifeline launched to replace the old 1-800-273-TALK system
-
Faith-based and veteran services fill care gaps for specific populations
-
Peer support groups (e.g., AA, NA, grief groups) offer non-clinical community help
These alternatives are especially critical in rural and low-income areas.
Technology Expanding Access
The rise of telehealth and mental health apps has opened new doors:
-
Online therapy platforms (e.g., BetterHelp, Talkspace)
-
Telepsychiatry for medication management
-
Mental wellness apps (e.g., Calm, Sanvello, Moodpath)
-
AI chatbots for first-line emotional support
-
EHR integration for better care tracking
These tools help people avoid long commutes, access specialized care, and feel less stigma—especially important for those managing care quietly.
Policy Momentum: Where the System Is Moving
Recent changes in law and funding are aimed at fixing the system:
-
Parity Enforcement: Holding insurers accountable for treating mental health like physical health
-
Certified Community Behavioral Health Clinics (CCBHCs): Federally funded centers offering walk-in services and coordinated care
-
988 Expansion: Easier access to mental health crisis support
-
Telehealth Protection Laws: Preserving access post-COVID
-
State Mental Health Task Forces: Targeted investments in workforce development and crisis response
Still, more investment is needed to train providers, modernize facilities, and reduce red tape for people seeking help.
Mental health support is no longer optional. It’s essential. From therapy and medication to peer support and crisis care, a functioning mental health system saves lives, reduces suffering, and strengthens communities.
As demand rises, so must commitment—from policymakers, health systems, schools, and employers. A well-supported mental health system doesn’t just heal—it prevents harm, fosters resilience, and builds a stronger nation.