In emergency medicine, seconds can mean the difference between life and death. Whether it’s a cardiac arrest, stroke, trauma, or natural disaster, the response time and tools used in those crucial moments determine outcomes.
Thanks to a wave of modern innovation, healthcare professionals now have access to technologies that dramatically improve survival and recovery rates. This article explores the most impactful emergency innovations currently saving lives in the U.S., their adoption trends, and what the future may hold.
Life-Saving Emergency Innovations and Impact Scores
Innovations That Save Lives in Emergencies
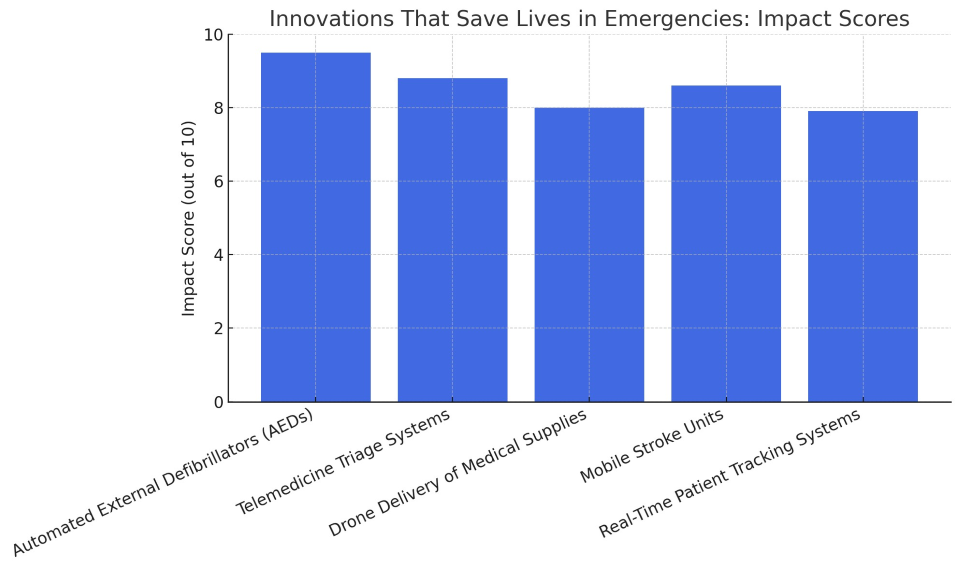
The chart above illustrates the relative impact of these technologies, with AEDs and mobile triage systems leading the charge in saving lives during critical moments.
1. Automated External Defibrillators (AEDs)
Impact Score: 9.5/10
AEDs are portable devices used to restore normal heart rhythm in people experiencing sudden cardiac arrest (SCA). They analyze heart rhythm and deliver a shock if needed—no medical training required.
Why It Saves Lives:
-
Increases survival rates up to 70% if used within 3 minutes
-
Widely available in public spaces (schools, gyms, airports)
-
Can be used by bystanders before EMS arrival
Key Fact: Over 350,000 people experience out-of-hospital cardiac arrest in the U.S. every year, and AEDs are one of the most effective interventions available.
2. Telemedicine Triage Systems
Impact Score: 8.8/10
During emergencies, determining who needs care first is vital. Telemedicine triage platforms allow remote clinicians to assess patients via video or app, prioritize cases, and dispatch the appropriate response.
Benefits:
-
Reduces ER overcrowding
-
Enables rural or understaffed facilities to triage remotely
-
Improves coordination during mass casualty incidents
-
Saves time in disaster scenarios (wildfires, hurricanes)
Hospitals and EMS systems that use tele-triage have reported up to 20% improvement in patient flow and faster access to high-acuity care.
3. Mobile Stroke Units
Impact Score: 8.6/10
A stroke patient loses nearly 2 million brain cells per minute. Mobile stroke units are specialized ambulances equipped with on-board CT scanners, lab testing, and tele-neurology consultation to deliver stroke treatment before arriving at the hospital.
Results:
-
Cut “door-to-treatment” time by up to 40 minutes
-
Increase eligibility for clot-busting drugs like tPA
-
Reduce disability rates and improve long-term recovery
These units are in use in major cities like Houston, New York, and Cleveland, and expanding rapidly.
4. Drone Delivery of Medical Supplies
Impact Score: 8.0/10
Drones are revolutionizing emergency logistics by delivering:
In rural or disaster-struck areas, drones can cut delivery times from hours to minutes, providing life-saving materials when roads are blocked or too far.
Real-World Example:
In North Carolina, Zipline drones have reduced emergency medication delivery times by over 50%, serving hospitals and clinics with minimal infrastructure.
5. Real-Time Patient Tracking Systems
Impact Score: 7.9/10
When patients are moved between ambulances, ERs, and ORs, delays and miscommunication can cost lives. Real-time tracking platforms allow:
-
Instant updates on patient status and location
-
Faster transfers between departments
-
Accurate ETA for trauma and cardiac teams
-
Integration with EHRs for continuous monitoring
Hospitals with robust tracking systems report fewer delays, better coordination, and higher survival rates during time-sensitive emergencies.
Other Emerging Innovations Worth Watching
While not yet as widespread, these innovations are on the horizon:
-
AI-Powered Early Warning Systems: Predict cardiac arrest or sepsis hours in advance
-
Smart Wearables: Alert EMS in real time for falls, arrhythmias, or diabetic crises
-
Smart Traffic Routing for EMS: Automatically adjusts traffic lights to speed up ambulances
-
Portable Ultrasound Devices: Used in ambulances for trauma and internal bleeding assessment
These tools are already showing promise in pilot programs and may become standard in the next decade.
How These Innovations Work Together
Imagine this real-world scenario:
A man collapses in a public park. A bystander uses an AED within 2 minutes. 911 dispatch receives the alert and sends a mobile stroke unit after a video triage identifies stroke symptoms. A drone brings a backup defibrillator and epinephrine in case of anaphylaxis. The patient’s real-time vitals are streamed to the ER via a wearable monitor.
This is not science fiction. This is 2025 healthcare, and it’s already happening in parts of the U.S.
Challenges and Barriers to Adoption
Despite their promise, emergency innovations face challenges:
-
Cost: High initial investment for tech like mobile stroke units or tracking systems
-
Training: EMS and hospital staff need time and resources to learn new systems
-
Integration: Systems must sync with existing infrastructure and EHRs
-
Regulation: Drones and AI platforms must meet strict healthcare safety standards
-
Access Equity: Urban centers benefit first—rural areas often lag behind
Still, public-private partnerships and federal grants are helping bridge these gaps.
Who’s Leading the Way?
Organizations and institutions pioneering life-saving innovations:
-
American Heart Association – Advocating AED training and placement
-
NIH and CDC – Funding mobile health pilots
-
Zipline and UPS – Leading drone logistics
-
City EMS Departments – Launching AI dispatch and tele-triage
-
Academic Hospitals – Testing AI and smart monitors in trauma centers
These collaborations are reshaping emergency care faster than ever.
Technology is transforming what’s possible in emergency care. With faster diagnosis, smarter routing, better tracking, and remote intervention tools, lives that might have been lost just a few years ago are now being saved.
But innovation alone isn't enough—it must be accessible, well-integrated, and trusted by providers. The more we invest in the tools that work, the more lives we can save when seconds count the most.