Pulse oximetry is a non-invasive, fast, and essential tool used to measure oxygen saturation (SpO2) in a person's blood. Especially during the COVID-19 pandemic, it became a household name—but this technology has long played a central role in hospitals, emergency services, and chronic care management.
This article takes a deep dive into pulse oximetry: what it is, how it works, its benefits and limitations, and where it fits into the future of healthcare in the U.S. We’ll also examine its accuracy across various conditions and discuss recent debates about racial bias and technology reliability.
What Is Pulse Oximetry?
Pulse oximetry is a technique used to estimate the percentage of oxygenated hemoglobin in the blood. The device, called a pulse oximeter, is typically clipped to a finger and uses light wavelengths to measure oxygen saturation without drawing blood.
Key Metrics:
The device uses red and infrared light to assess how much oxygen is in the blood. The amount of light absorbed varies based on how oxygenated the hemoglobin is, and this allows the device to compute saturation levels in real-time.
Clinical Applications of Pulse Oximetry
Pulse oximetry is used in a wide range of medical settings:
1. Emergency and Surgical Settings
Anesthesiologists use it during surgeries to monitor oxygen levels under anesthesia. EMTs and paramedics rely on it in ambulances to assess patient status quickly.
2. Chronic Disease Management
Patients with COPD, asthma, or heart failure often use pulse oximeters at home to detect early signs of decompensation.
3. COVID-19 Monitoring
During the pandemic, pulse oximeters became essential tools for managing mild COVID-19 cases at home, helping identify “silent hypoxia” before symptoms worsened.
4. Sleep Studies
Pulse oximeters are used in sleep labs and at home to diagnose sleep apnea, often alongside other sensors during overnight testing.
Advantages of Pulse Oximetry
Because of its simplicity and safety, pulse oximetry is used across all age groups—from newborns to the elderly.
Limitations and Accuracy Considerations
Despite its strengths, pulse oximetry has limitations. Certain conditions can reduce its accuracy, including:
Estimated Accuracy of Pulse Oximeters by Condition
Racial Bias and Equity in Pulse Oximetry
One of the biggest stories in healthcare technology recently has been the racial bias in pulse oximeter accuracy. Studies published in major medical journals revealed that pulse oximeters tend to overestimate oxygen levels in patients with darker skin tones, potentially delaying critical care.
In 2022, the FDA launched a formal review, and by 2024, recommendations were updated to emphasize:
-
Use of multi-wavelength sensors
-
Development of AI-assisted calibration
-
Greater representation in device testing populations
Hospitals are being encouraged to consider these limitations when interpreting results, especially for non-white patients.
Technological Innovations
The market is now responding to these concerns and opportunities with new developments:
1. Multi-Sensor Pulse Oximeters
Devices that combine pulse oximetry with perfusion index and plethysmographic waveform readings provide a more robust clinical picture.
2. Wearable Integration
Smartwatches like the Apple Watch and Fitbit now include SpO2 monitoring, enabling passive data collection during sleep or exercise.
3. Smartphone-Connected Oximeters
Bluetooth-enabled devices can sync data directly to patient portals or electronic medical records for remote monitoring.
4. AI & Predictive Modeling
Some startups are integrating oxygen saturation data with machine learning to predict deteriorations in chronic patients days before they show symptoms.
Accuracy of Pulse Oximetry Across Patient Conditions
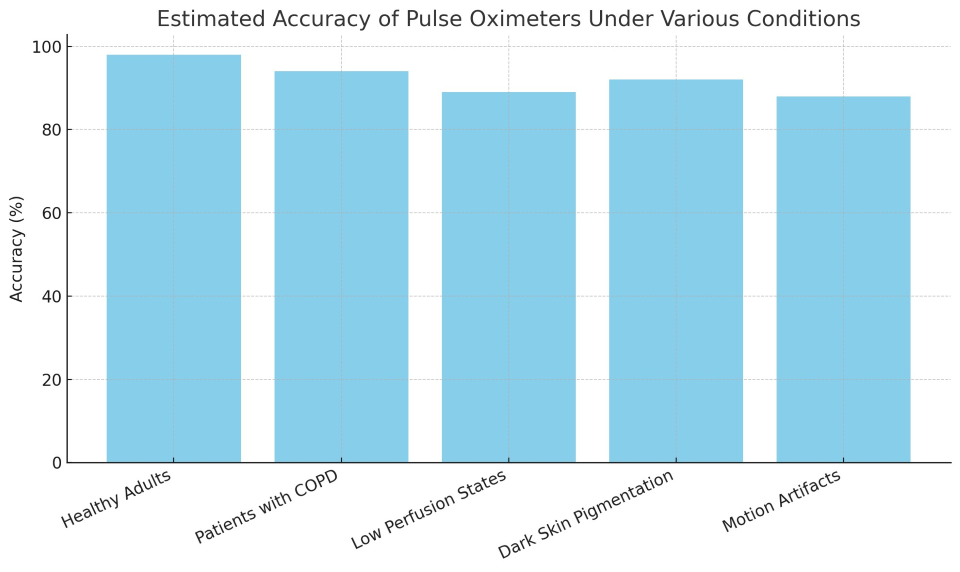
As the chart shows, while accuracy remains high in healthy patients, it drops in motion-affected or low-perfusion states. These differences, though seemingly small, can lead to major consequences in clinical decision-making, especially in critically ill patients.
Home Monitoring: Empowering Patients
The availability of over-the-counter pulse oximeters has allowed millions of Americans to monitor their health at home. However, proper education is crucial:
Best Practices:
Pharmacists and primary care providers are encouraged to educate patients on how to use these tools effectively.
Regulation and FDA Oversight
As of 2024, the FDA has:
-
Issued new draft guidance on pulse oximeter labeling
-
Urged manufacturers to submit racial subgroup data in approval processes
-
Proposed performance minimums under varied conditions (motion, pigmentation, perfusion)
Consumers are also advised to check for FDA-cleared models, particularly if used for home chronic disease monitoring.
Pulse oximetry has become a symbol of modern healthcare: accessible, high-tech, and empowering. Yet like all tools, it is only as good as its context. Understanding its limitations—especially for patients of color and those with circulation challenges—is essential for fair and accurate care.
As innovation continues, the goal must be not only better sensors, but smarter interpretation and equitable design.