In the U.S. healthcare system, quality care depends on teamwork. Doctors, nurses, therapists, and administrative staff must all work in sync. What makes this happen is staff coordination—the behind-the-scenes effort that ensures everyone knows their role, responsibilities, and timing.
Staff coordination is about aligning people, processes, and communication. It determines whether care is seamless or scattered, whether patients feel supported or frustrated. In a system that’s under constant pressure from staffing shortages, rising costs, and patient expectations, effective coordination is a make-or-break factor.
Let’s unpack what staff coordination is, why it’s so critical in the U.S., and how it's being implemented and improved.
What Is Staff Coordination?
Staff coordination is the organized effort to manage, communicate, and deploy healthcare workers to ensure timely, safe, and efficient care delivery. It covers a wide range of tasks:
-
Scheduling shifts and on-call rotations
-
Assigning responsibilities based on skill level
-
Managing communication between departments
-
Tracking patient handoffs and transitions
-
Resolving staffing conflicts or emergencies
-
Ensuring compliance with labor laws and healthcare regulations
At its core, it’s about making sure the right person is in the right place, at the right time, with the right tools and information.
Why Staff Coordination Matters in U.S. Healthcare
1. Patient Outcomes Depend on Teamwork
Poor coordination often leads to miscommunication, delays in treatment, and medical errors. A missed lab result, an uncommunicated medication change, or a patient left waiting for transport—these all stem from coordination breakdowns.
Conversely, tight coordination ensures that care teams can respond quickly, prioritize critical needs, and deliver consistent care. Studies show hospitals with better interprofessional coordination have lower readmission rates and better post-discharge outcomes.
2. Healthcare Worker Burnout Is a Real Crisis
In 2023, over 60% of U.S. nurses reported burnout. One major factor? Staffing mismanagement. When shifts are unbalanced, responsibilities unclear, or communication sporadic, staff morale tanks.
Good coordination systems ensure fair shift distribution, clearer expectations, and better support. That translates directly to job satisfaction and retention.
3. Costs Are Sky-High—Coordination Can Help
Healthcare labor is expensive. Overtime, temp staff, and inefficiencies drive up costs. Coordination tools—like centralized scheduling platforms and predictive staffing models—help allocate resources more efficiently. Fewer last-minute gaps mean lower costs and better coverage.
Who Coordinates Staff—and Where?
Staff coordination looks different depending on the setting. Here’s a breakdown:
[See Table Above]
Each coordinator role is essential to maintaining workflow, handling staffing challenges, and keeping patient care smooth. Whether it’s a Charge Nurse covering a night shift or a Clinic Manager rerouting patients during flu season, the goal is the same: keep care flowing without friction.
Coordination Efficiency Translates Into Patient Satisfaction
Let’s look at the relationship between how well staff are coordinated and how satisfied patients are:
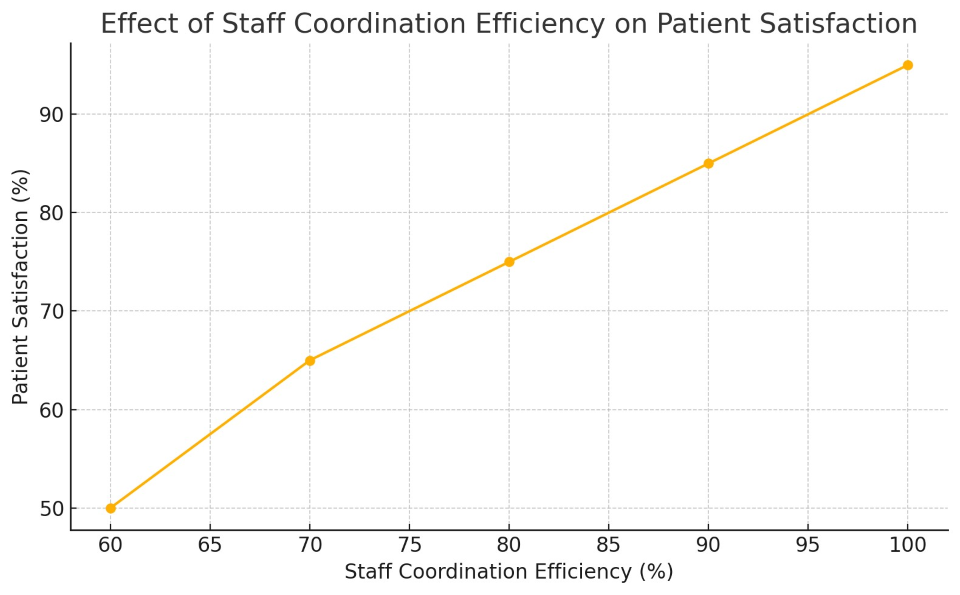
As this chart shows, there’s a direct connection. As coordination efficiency improves, patient satisfaction rises. In fact, once efficiency surpasses 80%, satisfaction levels soar. This isn’t just theoretical—real-world surveys like HCAHPS reflect this pattern.
Real-World Coordination Scenarios in U.S. Health Systems
A. Emergency Departments
In busy ERs, coordination is life or death. Bed assignments, triage, diagnostics, and consults must be timed precisely. Hospitals like the Mayo Clinic use real-time tracking systems and shift huddles every few hours to ensure roles are clear and patient flow is optimized.
B. Post-Acute Care Transitions
After a hospital discharge, patients often transition to skilled nursing, rehab, or home care. Poor coordination during this transition is a major reason for 30-day readmissions. Kaiser Permanente and Geisinger have both implemented case management systems where nurses or social workers oversee every discharge to ensure follow-ups are scheduled and patient instructions are clear.
C. Outpatient Clinics
In clinics, staff coordination means managing appointment slots, lab tests, provider availability, and equipment access. Large systems like Cleveland Clinic use advanced scheduling software with AI that accounts for no-show rates and patient needs to better align staffing.
Common Challenges in U.S. Staff Coordination
Despite its importance, staff coordination in the U.S. health system faces some serious roadblocks:
1. Technology Gaps
Many healthcare organizations still use outdated scheduling systems or even paper logs. Lack of EHR integration means information isn’t shared in real time across departments, leading to confusion and delays.
2. Staffing Shortages
Shortages make even the best coordination plans difficult. When there simply aren’t enough nurses or aides, coordinators scramble to fill gaps—often leading to burnout or errors.
3. Fragmentation of Care
Especially in rural areas or among patients with multiple providers, coordination between hospitals, clinics, and specialists can be weak. Interoperability remains a major barrier.
4. High Turnover Rates
When staff turnover is high, especially in long-term care or community health, continuity suffers. New staff constantly need training, and experienced coordinators are in short supply.
Solutions: How the System Is Responding
Here’s how U.S. health systems are trying to fix coordination issues:
The Future of Staff Coordination
Expect to see smarter, more integrated systems moving forward:
-
AI and Machine Learning will predict staffing needs and automate schedules.
-
Real-Time Dashboards will show staff availability, patient flow, and bottlenecks.
-
Cross-Training will make teams more flexible and capable of adjusting quickly.
-
Decentralized Coordination (e.g., via mobile apps) will empower frontline staff to self-adjust in real-time.
As healthcare continues to evolve, so will the ways we manage the teams behind it.
Staff coordination isn’t just a logistical task—it’s a cornerstone of modern healthcare. In the U.S., where care is fragmented, demand is high, and staff are stretched thin, good coordination can be the difference between thriving and struggling.
From faster treatment times and smoother transitions to happier staff and patients, the payoff is real. As systems embrace better tools and smarter practices, staff coordination will become not just more efficient—but more human-centered and resilient.