The United States is home to more than 45 million immigrants, representing about 14% of the nation’s population. These individuals and families come from diverse backgrounds, bringing unique strengths—and facing unique challenges—when navigating the U.S. healthcare system.
Whether newly arrived or long established, many immigrants struggle to access the healthcare services they need due to language barriers, financial limitations, or immigration status concerns. This article explores which services are most commonly used, what obstacles exist, and how support systems are working to improve care access for this growing population.
Healthcare Services Accessed by Immigrants
Most Accessed Healthcare Services by Immigrants
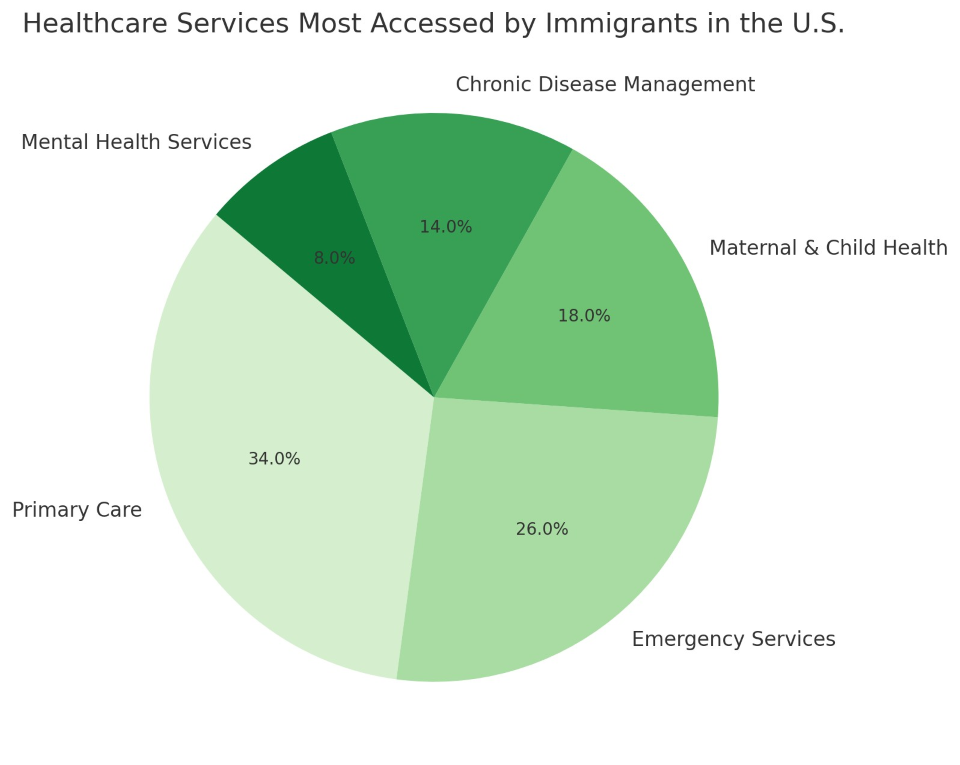
As the chart shows, primary care and emergency services are the two most commonly accessed health services among immigrants in the U.S., followed by maternal and child health, chronic disease management, and mental health services—which remains underutilized in many immigrant communities.
Why Access Matters
Healthcare access directly impacts the long-term health, financial stability, and productivity of immigrant communities. When preventive care is missed, minor conditions can worsen into major ones, leading to costlier treatments, poorer outcomes, and increased emergency room use.
Access isn’t just about having a doctor nearby—it includes:
Primary Care: The Most Essential Touchpoint
Primary care is often the first—and sometimes only—form of regular healthcare that immigrants receive. It covers:
Many immigrants rely on community health centers (CHCs) or Federally Qualified Health Centers (FQHCs), which offer low-cost or sliding-scale fees and multilingual staff.
Emergency Services: The Last Resort for Many
Due to lack of insurance or access to regular care, immigrants often turn to emergency rooms when health problems escalate. Under EMTALA, hospitals must provide emergency treatment to anyone, regardless of immigration status or ability to pay.
However, relying on emergency services leads to:
Maternal and Child Health Services
Women and children make up a significant portion of immigrant communities. Services often used include:
Programs like WIC (Women, Infants, and Children) and Medicaid (in eligible states) help cover these services, though awareness and eligibility vary.
Chronic Disease Management
Conditions like diabetes, hypertension, and high cholesterol are prevalent among many immigrant groups due to diet changes, stress, and limited preventive care in their countries of origin.
Yet, immigrants are less likely to receive consistent management or regular follow-ups for these conditions due to:
Mental Health: The Hidden Crisis
While mental health conditions affect people across all backgrounds, immigrants often face:
-
Stigma associated with therapy or mental illness
-
Isolation and trauma, especially among refugees
-
Fear of sharing personal information
-
Lack of culturally competent providers
This leads to significant underutilization of counseling, psychiatry, and crisis support—even among those who have experienced severe trauma or displacement.
Legal and Documentation Barriers
Immigrants with undocumented status often hesitate to seek care, even when eligible. Reasons include:
-
Fear of being reported to immigration authorities
-
Confusion about what services are available
-
Myths that seeking care could affect immigration status (e.g., green card applications)
In truth, healthcare providers are not allowed to share patient information with immigration enforcement under HIPAA laws, and public hospitals and clinics do not check immigration status for emergency care or many basic services.
Common Care Access Points for Immigrants
These resources serve as the frontline of immigrant healthcare, especially in cities and states with high immigrant populations.
Technology and Outreach Solutions
Digital tools are helping bridge healthcare gaps for immigrants:
-
Telehealth platforms with interpretation services
-
Text-based appointment reminders in multiple languages
-
AI-driven symptom checkers with language options
-
Community WhatsApp groups sharing healthcare resources
-
Digital flyers and websites explaining benefits eligibility
When combined with on-the-ground outreach, these tools improve health literacy and reduce missed appointments.
Policy and Protections
Key policies that help immigrants access care:
-
EMTALA: Emergency services are guaranteed for all
-
CHIP & Medicaid (for children in many states): Covers children regardless of parental status
-
Public Charge Rule (2022 rollback): Applying for Medicaid or food assistance does not impact immigration applications
-
Language Access Mandates: Healthcare providers receiving federal funds must offer interpretation
Still, there are inconsistencies across states. Some states extend Medicaid-like coverage to undocumented immigrants for pregnancy and childhood services; others do not.
Improving the System: What’s Needed
To close the care gap, experts recommend:
-
Expanding state-funded health programs for all income-eligible residents
-
Increasing the number of multilingual healthcare providers
-
Funding trusted community health workers (CHWs) from immigrant communities
-
Removing administrative barriers from safety-net programs
-
Supporting education campaigns in immigrant media and local networks
Immigrants in the U.S. deserve the same quality and dignity in healthcare as anyone else. While access has improved in some areas, barriers still prevent millions from receiving the basic care they need to live healthy lives.
Through inclusive policy, community support, culturally aware providers, and smart outreach, the U.S. can build a system where no one fears walking into a clinic—and everyone leaves with help.