Electronic Health Records (EHRs) are digital versions of patients’ paper charts, but they’re much more than that. They provide a comprehensive view of a patient’s medical history, lab results, medication list, treatment plans, allergies, imaging, and more—all in one place. In the U.S., where healthcare is highly fragmented and heavily regulated, EHRs are essential for managing patient data efficiently, securely, and accurately.
EHRs: A Solution to a Complicated System
The U.S. healthcare system is massive, with over 6,000 hospitals, hundreds of thousands of physicians, and a mix of public and private insurers. Historically, patient records were stored in paper files, scattered across clinics and departments. That led to fragmented care, duplicate tests, and preventable medical errors.
EHRs emerged as a solution to these inefficiencies. They’re designed to streamline communication between providers, reduce mistakes, and improve care coordination. Since the 2009 HITECH Act, the U.S. government has pushed hard for nationwide EHR adoption, offering billions in incentives to providers who transitioned from paper to digital systems.
EHR vs. EMR: Know the Difference
Though often used interchangeably, Electronic Health Records (EHRs) and Electronic Medical Records (EMRs) are not the same:
-
EMR refers to digital records within a single practice. Think of it as a digital version of a patient chart used by one doctor.
-
EHR, on the other hand, is more holistic. It includes data from multiple sources—primary care, specialists, hospitals, labs—and is built to be shared across settings.
If you’re a patient, the EHR is what follows you from your general practitioner to your cardiologist and back. That continuity can make a huge difference in diagnosis, treatment, and long-term health outcomes.
Key Features of an EHR
A robust EHR system includes:
-
Medical history and demographics
-
Lab and imaging results
-
Medication and allergy lists
-
Immunization records
-
Progress notes
-
Clinical decision support (CDS) tools
-
Secure communication between patients and providers
-
Billing and insurance data integration
Some advanced systems also integrate telemedicine platforms, patient wearables, and AI-driven analytics to support diagnosis and risk prediction.
Benefits of EHRs in the U.S. System
The U.S. has unique challenges—patients often see multiple providers across different health systems. EHRs help unify that care.
Here’s a breakdown of the core benefits:
EHR Adoption Trends
Adoption has increased rapidly over the past decade, especially after the HITECH Act tied Medicare/Medicaid payments to “Meaningful Use” of EHRs. Here’s what the growth looks like:
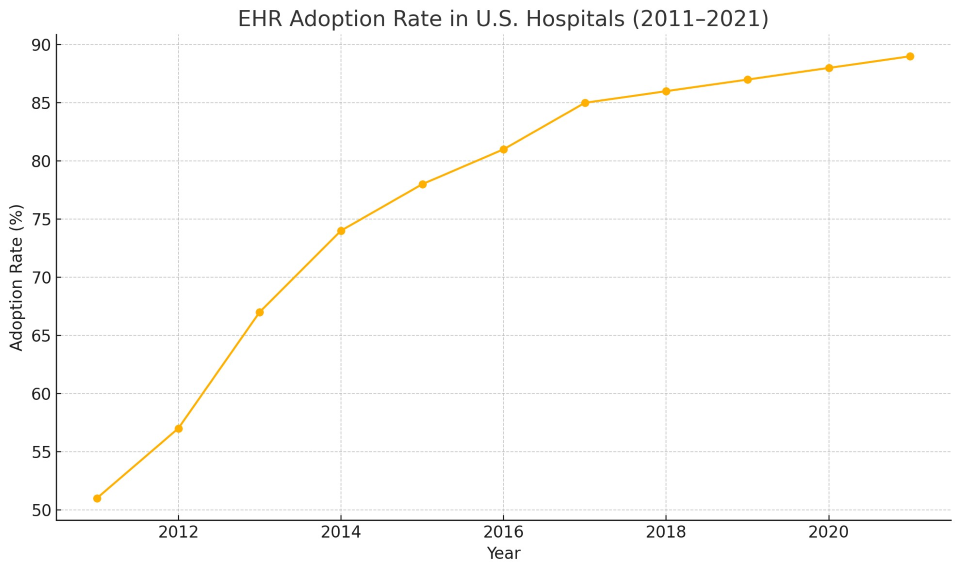
From 2011 to 2021, the percentage of U.S. hospitals using certified EHRs rose from just over 50% to nearly 90%. Smaller practices and rural clinics have historically lagged behind, but adoption is catching up thanks to cloud-based systems and mobile-friendly platforms.
Use Case: How EHRs Improve Real Patient Care
Imagine a patient with diabetes who sees a primary care doctor, an endocrinologist, and a podiatrist. Before EHRs, each provider might have kept separate, paper-based charts, with no visibility into the others’ treatment plans. That disjointed approach could lead to overlapping prescriptions, conflicting advice, or gaps in monitoring.
With a shared EHR, all three providers can see the full picture—lab values, previous prescriptions, lifestyle notes, even messages the patient sent through their portal. They can collaborate in real-time, even across systems, using secure messaging and shared care plans. That’s the kind of coordination that prevents complications and saves lives.
The Drawbacks: What’s Not Working Yet
Despite the promise, EHRs haven’t solved every problem. Here are the most common challenges:
1. Interoperability
One of the biggest issues is that many EHR systems still don’t communicate well with others. A patient’s data may be stored in multiple systems that can't share information. This lack of “interoperability” results in continued fragmentation.
2. Cost
Implementing a high-quality EHR system can cost anywhere from tens of thousands to millions of dollars, depending on the size of the organization. Even with federal aid, small practices often struggle to afford it.
3. Usability and Workflow Issues
Many doctors say they spend more time clicking through EHR screens than talking to patients. Poorly designed interfaces and excessive data entry contribute to clinician burnout, one of the most pressing problems in healthcare today.
4. Cybersecurity Risks
With digitized records comes the risk of hacking. Healthcare data breaches have been increasing year over year, leading to legal and financial consequences for providers—and anxiety for patients.
What’s Next: The Future of EHRs
The evolution of EHRs is far from over. Here’s what’s on the horizon:
-
AI Integration: Clinical decision tools powered by AI will help flag risks, recommend treatments, and catch errors.
-
Patient-Generated Data: Integration with wearables (like Apple Watch, Fitbit) will enrich EHRs with real-time health metrics.
-
Mobile Access: More providers and patients are using smartphones and tablets to view or update health records.
-
Cloud Computing: Cloud-based EHRs reduce costs, improve scalability, and support remote care teams.
-
FHIR Standards: The Fast Healthcare Interoperability Resources (FHIR) initiative is creating standardized ways for different systems to share data.
EHRs are a cornerstone of modern healthcare in the U.S. They’ve helped digitize, centralize, and streamline care across an incredibly complex system. While issues like interoperability and usability still need work, the benefits are real: better care coordination, fewer errors, and more empowered patients.
As we move into a more connected, data-driven era of healthcare, the focus should shift from simply using EHRs to using them well—in ways that support clinicians, protect patients, and make the entire system smarter and more humane.