In the fast-evolving landscape of American healthcare, medical directors are vital change agents who balance patient care with organizational leadership. Whether they work in hospitals, health plans, or long-term care, their role combines deep clinical knowledge with sharp administrative acumen.
This article dives into what medical directors do, how their responsibilities vary across specialties and settings, and how trends like telehealth, data analytics, and physician burnout are reshaping their leadership in 2025 and beyond.
Who Is a Medical Director?
A medical director is a licensed physician responsible for overseeing clinical services, improving healthcare quality, and aligning operations with medical standards. They often act as the bridge between frontline clinical staff and executive management, making high-level decisions that directly affect patient outcomes and provider well-being.
Common Work Environments:
-
Hospitals and integrated health systems
-
Ambulatory surgical centers
-
Behavioral health and substance abuse facilities
-
Skilled nursing and long-term care settings
-
Insurance companies and health maintenance organizations (HMOs)
-
Public health agencies and telemedicine platforms
Core Responsibilities of a Medical Director
Medical directors wear many hats. Some of their key functions include:
1. Clinical Oversight
They monitor practice patterns, develop clinical protocols, and ensure alignment with evidence-based standards of care.
2. Regulatory and Legal Compliance
They manage audits, ensure HIPAA adherence, and help organizations pass inspections by The Joint Commission or CMS.
3. Provider Performance & Peer Review
Medical directors lead performance evaluations, handle conflict resolution, and implement quality improvement initiatives across departments.
4. Education and Credentialing
They facilitate onboarding, continuing education, and credentialing processes for physicians and mid-level providers.
5. Strategic Development
From launching new service lines to integrating technology, medical directors collaborate with C-suite leaders on long-term strategy.
Training and Credentials Required
How to Become a Medical Director:
-
Medical Degree: MD or DO from an accredited institution
-
Clinical Experience: At least 5–10 years in a leadership or attending role
-
Administrative Training: Many pursue an MBA, MHA, or MPH
-
Certifications: Examples include Certified Physician Executive (CPE) or Certified Medical Director (CMD) for post-acute care
Physicians with strong communication skills, systems thinking, and experience in multidisciplinary environments often make the best candidates.
A Day in the Life: What Do Medical Directors Actually Do?
Here’s a sample daily schedule for a hospital-based medical director:
Not every director sees patients daily, but many do, especially in smaller organizations.
Specialty Comparison: Salary vs. Administrative Hours
Administrative workload and compensation often vary by specialty. Some roles require more back-office oversight, while others involve hands-on leadership.
Salary vs Admin Hours by Specialty
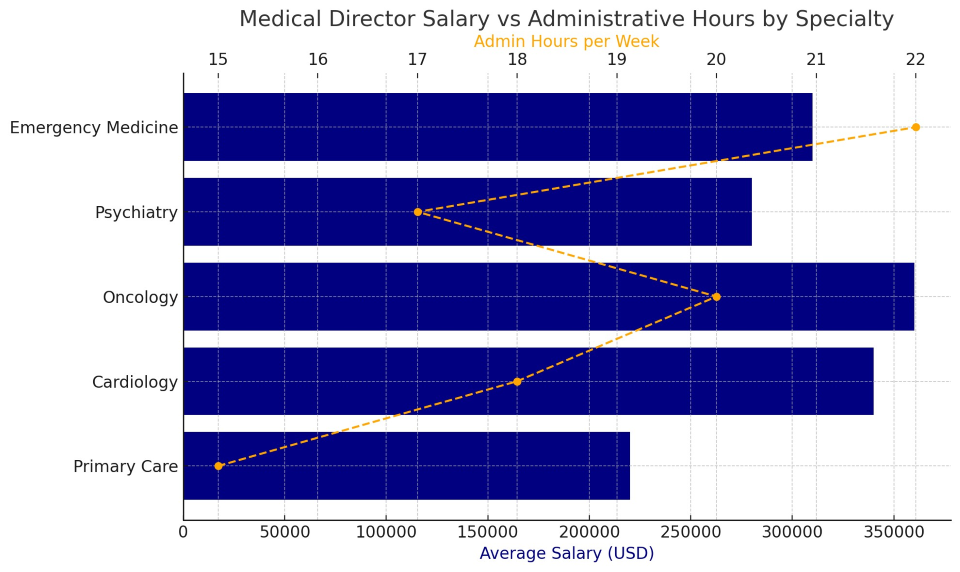
The chart above illustrates how fields like oncology and emergency medicine often demand more administrative time due to the complex, multidisciplinary nature of their care environments.
Leadership and Ethical Tensions
Medical directors are often caught in the middle of clinical and corporate priorities. Examples include:
-
Pushing throughput targets while maintaining safe patient loads
-
Approving budget cuts that affect staff morale
-
Managing underperforming clinicians who are otherwise well-liked
-
Balancing cost savings with expensive but life-saving treatments
The best medical directors lead with transparency, ethics, and a focus on long-term trust—not just short-term metrics.
Case Example: Strategic Leadership in a Community Hospital
Name: Dr. Rosa Mitchell
Position: Medical Director, Rural Health Network in Nebraska
Challenges: High staff turnover, outdated EHR, rising sepsis rates
Initiatives:
-
Introduced sepsis protocols and nurse alerts
-
Secured a grant to upgrade to a new cloud-based EHR
-
Developed a leadership pipeline for in-house provider promotions
Results: 19% drop in clinical error rate and improved patient satisfaction scores in under 12 months.
Performance Metrics: How Success Is Measured
Medical directors are evaluated based on both qualitative and quantitative factors:
Common KPIs:
-
Hospital-acquired infection rates
-
Physician retention and satisfaction
-
Patient readmission rates
-
Documentation accuracy
-
Time to credential new hires
-
Patient experience (HCAHPS) scores
In payer settings, metrics like utilization rates, claims adjudication times, and clinical appropriateness reviews come into play.
The Role in Healthcare Innovation
Today’s medical directors are expected to lead innovation in:
-
AI adoption for clinical decision support
-
Telehealth integration for remote populations
-
DEI strategy in clinical workforce and patient outreach
-
Climate resilience for healthcare infrastructure
-
Staff wellness initiatives amid nationwide burnout
They also guide the ethical use of data, ensuring AI tools and digital health platforms enhance care without compromising patient trust.
The modern medical director is more than just an administrator—they are architects of clinical culture. With responsibilities ranging from credentialing and compliance to policy and patient safety, they represent a new generation of physicians who lead from both the head and the heart.
As medicine grows more complex, the role of the medical director becomes not just essential—but transformational.