A Critical Leadership Role in U.S. Healthcare
In the fast-moving world of healthcare, one role stands at the intersection of patient care, staff performance, and regulatory compliance: the Director of Nursing (DON). In the U.S. healthcare system, this role is vital to ensuring that nursing departments function smoothly, meet legal standards, and deliver excellent care.
But the role isn’t just about keeping things in order. A Director of Nursing has the power to influence the culture, efficiency, and reputation of a facility. From large hospitals to long-term care homes, the DON ensures nurses are supported, patients are safe, and standards are met—or exceeded.
What Does a Director of Nursing Actually Do?
The DON is the top nurse leader in a facility. They bridge the clinical side of care with the administrative side. Their days might involve reviewing patient safety reports in the morning, meeting with HR about staffing in the afternoon, and responding to a regulatory audit by the evening.
Here's a quick breakdown of typical duties (see the table above for a more detailed list):
-
Supervise and evaluate nursing staff
-
Create and enforce nursing policies and procedures
-
Oversee staff schedules and department budgeting
-
Monitor patient care quality and outcomes
-
Ensure compliance with local, state, and federal healthcare laws
-
Manage hiring, onboarding, and continuing education for nurses
They’re also the point person when something goes wrong—whether it’s a medication error, staff shortage, or inspection issue.
How the Role Varies by Facility Type
While the core responsibilities are similar, how a DON operates depends on the setting.
1. Hospitals
In larger hospitals, the DON might be one of several nurse leaders and may oversee specific departments like ICU, pediatrics, or surgical units. The role is fast-paced and collaborative, involving many meetings and data-driven decisions.
2. Nursing Homes & Long-Term Care Facilities
Here, the DON often oversees the entire nursing function. These roles are heavily compliance-focused, with frequent audits and a need for tight documentation. Given the aging U.S. population, these facilities are under increasing scrutiny and demand.
3. Home Health Agencies
In this setting, the DON coordinates nurses working in the field. Logistics and communication skills are key, as care is delivered in patients’ homes. Ensuring quality and consistency when staff aren’t centralized is a major challenge.
Educational Pathway to Become a DON
To move into this role, nurses need both credentials and experience.
While some smaller facilities may hire a DON with a BSN and strong leadership background, most competitive positions require a master’s degree and formal management training.
Salary Insights Across the U.S.
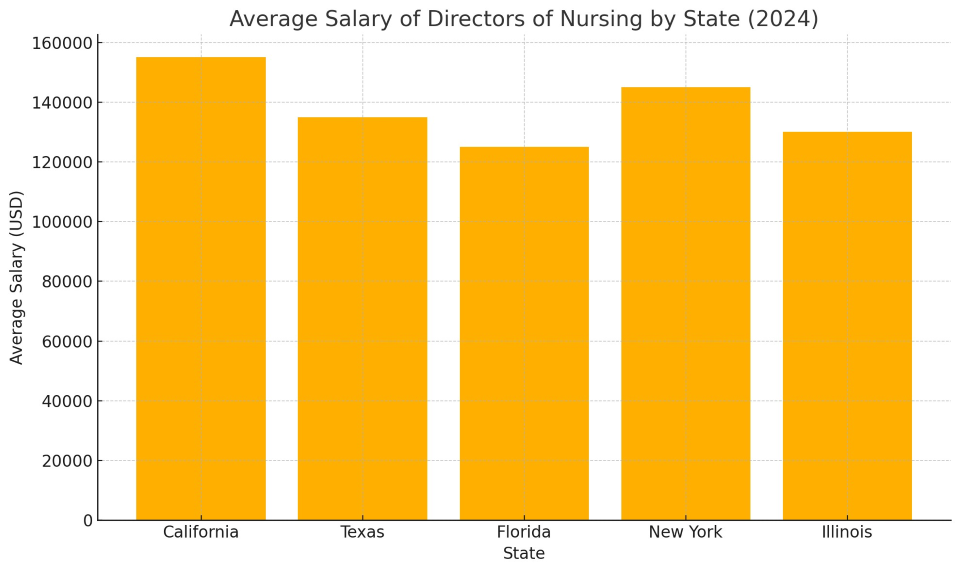
According to 2024 data, DON salaries range from $110,000 to over $160,000 depending on location and facility size. Salaries also reflect regional demand, cost of living, and facility funding.
Take a look at the graph below for a snapshot:
-
California leads due to its high cost of living and large healthcare systems.
-
Texas and Florida are competitive, especially in private systems or high-demand metro areas.
-
New York sees a split: very high pay in NYC, lower in rural upstate regions.
Real-World Challenges Facing Directors of Nursing
The position comes with significant pressure. Some of the biggest challenges DONs face include:
-
Nursing Shortages: Staffing shortages are rampant in post-COVID healthcare, forcing DONs to manage overworked teams and reduce burnout.
-
Compliance Overload: Healthcare is one of the most heavily regulated industries. DONs must stay on top of constant changes in CMS, OSHA, HIPAA, and state rules.
-
Budget Cuts: Many facilities face financial strain. DONs must often do more with less—cutting overtime, consolidating roles, and fighting for resources.
-
Litigation Risk: A single mistake or incident can result in lawsuits, especially in long-term care settings. Documentation and protocol adherence are essential.
Why the Role Matters More Than Ever
The U.S. healthcare system is undergoing major transformation. There’s an aging population, a shift toward value-based care, and a growing emphasis on patient satisfaction. The DON sits at the heart of these changes.
Here’s why the role is growing in importance:
-
Quality Scores Are Tied to Funding: Medicare and Medicaid reimbursement now depends on patient outcomes and quality metrics.
-
Technology Integration: As EHRs, telehealth, and AI tools spread, DONs must train staff and lead adoption.
-
Workforce Development: With Gen Z and Millennial nurses entering the workforce, expectations around flexibility, leadership style, and training have shifted. DONs have to adjust how they manage and mentor.
Advice for Aspiring Directors of Nursing
If you’re aiming for a DON position, here are a few practical steps:
-
Start with Strong Clinical Skills: Build a solid foundation in patient care, especially in acute or critical care settings.
-
Take on Leadership Roles: Volunteer for team lead positions, committee work, or staff education programs.
-
Get Certified: Pursue certifications like NE-BC or CDONA to demonstrate commitment and credibility.
-
Invest in Education: Consider an MSN or MBA in Healthcare Management.
-
Find a Mentor: Connect with current DONs or nurse executives who can offer guidance, feedback, and career insight.
The Director of Nursing is more than a job title—it’s a leadership role that carries real responsibility for people’s lives and livelihoods. In a fragmented, high-stakes healthcare system like the one in the U.S., strong nursing leadership isn’t optional—it’s essential.
For those ready to step up and lead with both compassion and competence, the role of DON offers a meaningful and challenging career path.